What are the challenges for getting gay men at risk of HIV to take PrEP?

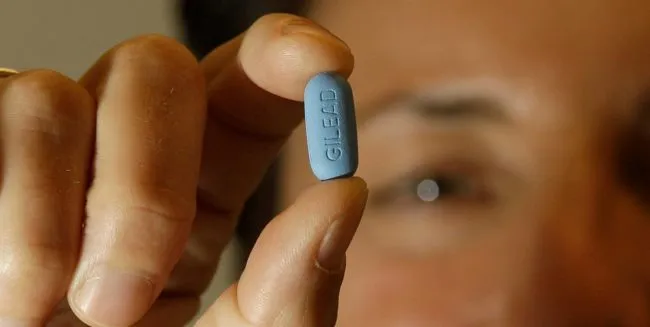
PrEP: Man holding a pill used for Pre-Exposure Prophylaxis (PrEP) to prevent HIV infection
Professor Rusi Jaspal and Dr Jake Bayley of De Montfort University explain their findings from conducting research into PrEP and the attitudes of gay men.
In 2012 Truvada, an anti-HIV drug, was approved by the Food and Drug Administration in the US.
Since then, many gay men with private health insurance in the States have been able to access this important prevention drug.
The story in England is much more complicated. After a long legal battle with the UK Government, PrEP has been funded in England for 10,000 at-risk patients only, a fraction of the total of those who need it. This has left many gay men seeking PrEP through other channels, such as buying a generic (or cheaper non-branded) version online, often without clinical support.

Last week it was announced that 56 Dean Street, Europe’s busiest sexual health clinic, had launched a ‘PrEP Shop’ to provide access to generic PrEP. It will cost £55 per month allowing more gay men to access PrEP, but only those who can afford it.
PrEP is really important. We’ve already seen the incredible benefits of PrEP in reducing new HIV infections. Public Health England data revealed a 40 percent decrease in new HIV diagnoses in England in 2016 compared to the year before.
This eye-watering fall in new diagnoses marked a significant shift in the HIV epidemic in Britain, given the year-on-year increase in new diagnoses that had been observed previously.
Yet, the high cost of PrEP is not the only barrier to PrEP. There are other social and psychological factors that can make it inaccessible to gay men.
In 2016, we interviewed a group of gay men in London and Leicester to find out what they knew and thought about PrEP. All of the participants reported either ‘cursory’ or no knowledge of PrEP prior to the study but, when it was explained to them, most saw PrEP as a good thing.
However, when asked whether they would use PrEP themselves, most expressed concerns.
PrEP
RELATED: What is PrEP and how can I get it?
There was uncertainty about whether PrEP would actually work and some men expressed fear that the drug might have long-term side-effects, despite being used for years in those living with HIV with few side effects.
Younger gay men thought PrEP would be effective in preventing HIV. However, older men thought that only condoms were an effective way of preventing HIV – unsurprisingly after years of public health messages advocating condom use.
Gay men may also worry that others will react badly to their use of PrEP, otherwise known as ‘slut shaming’. They may fear judgement from friends and family, and worry that their sexual partners might assume that they have HIV or that they like ‘bareback’ sex. PrEP stigma seems to put some men off.
Most interviewees just did not want to see themselves as ‘high risk’, a term that is often associated with PrEP use, even though many themselves reported engaging in behaviours that actually put them at high risk of acquiring HIV.
If you do not acknowledge that you are at risk of HIV, you are unlikely to take necessary steps to reduce your risk. It’s crucial that those gay men at risk of HIV actually acknowledge this and consider including PrEP in their risk reduction strategy.
We then conducted another survey of PrEP awareness in gay men in Leicester and found that 56 percent of those surveyed did not think that PrEP would be of personal benefit.

Those who correctly perceived themselves as high risk (i.e. those who barebacked regularly) and went for regular HIV tests (meaning a high level of sexual health knowledge and engagement) were much more likely to consider using PrEP.
Currently, most of the gay men who take PrEP are well informed about HIV risk, and they have knowledge of how to access it. Conversely, many of those who do not access PrEP have poor HIV knowledge and may be taking risks without being aware of this. Gay men from ethnic minority backgrounds are one such group.
So it is heartening to see that Public Health England’s HIV Innovation Fund has supported projects, such as our Sholay Love project, conducted in collaboration with NAZ Project London (a charity for supporting the sexual health of Asian, Black and Latino populations).
Sholay Love will raise awareness of HIV risk and prevention in South Asian gay and bisexual men, an underserved population in the world of sexual health to educate about the benefits of PrEP and engaging with sexual health services.
We aim to improve PrEP uptake in a group in which HIV infection rates have yet to see the dramatic fall seen in other groups. Only when all groups at risk of HIV have equitable access to PrEP will our goal of zero new HIV transmissions become a reality.

